We’ve compiled a repository of resources approved by our pediatric mental healthcare team. Let us know if you’d like some free printed materials by using our contact page.

Sign up to receive newsletters and updates.
Clinical Pearls and Guidelines support providers in managing mental and behavioral health disorders in youth. These
resources include information on how to assess for conditions, common misdiagnoses, treatment recommendations, and
monitoring of the condition. We would like to thank the Massachusetts Child Psychiatry Access Program for allowing us
to adapt these resources for South Carolina. Jump to: Anxiety, Autism, ADHD, Depression, OCD, PTSD.
Symptoms of anxiety include:
Symptoms of autism spectrum disorders include:
Symptoms of ADHD include:
Symptoms of depression include:
Symptoms of OCD include:
Symptoms of PTSD include:
Parent Medication Guides were developed by the American Academy of Child and Adolescent Psychiatry (AACAP) and the American Psychiatric Association (APA) to help a child and/or adolescents’ caregiver make informed decisions about treating mental disorders. We also offer NIMH brochures and fact sheets on mental disorders and related topics. Click the link to access electronic versions.
Inquire through the YAP-P Contact Page about receiving medication guides.
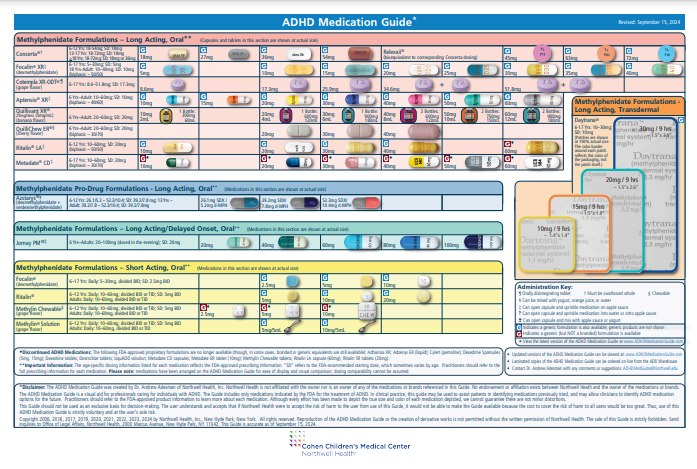
The ADHD Medication Guide© is a visual aid for professionals caring for individuals with ADHD. The guide provides dosing information and images of medications indicated for the treatment of ADHD by the FDA. In clinical practice, this guide may be used to assist patients in identifying medications previously tried and may allow clinicians to identify ADHD medication options for the future.
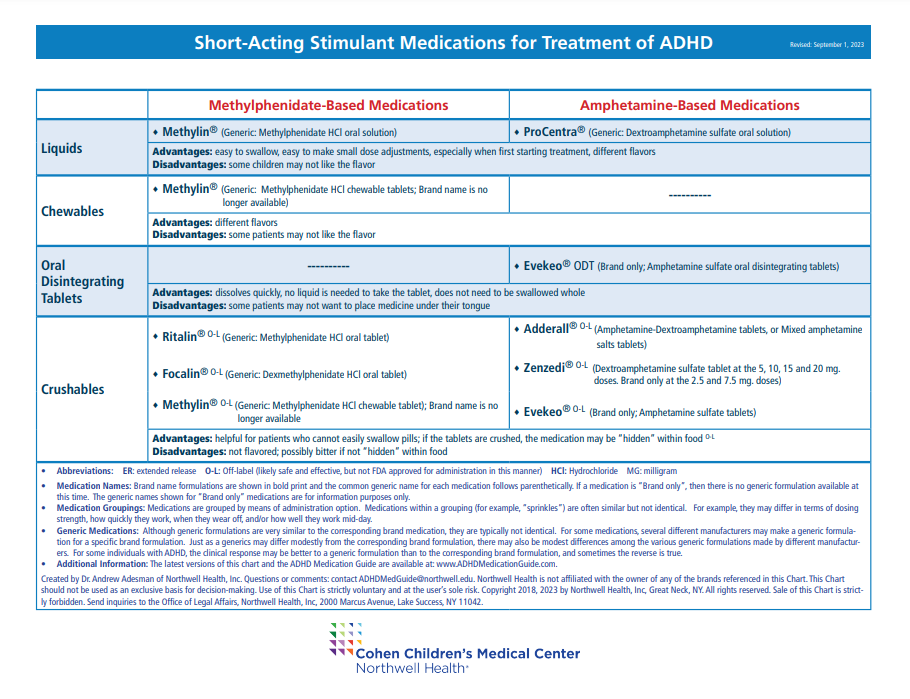
The Stimulant Medication Guide© is a visual aid for
professionals caring for individuals with ADHD. The
Guide shows short-acting and long-acting stimulant medications indicated for the treatment of ADHD organized by method of administration (liquids, sprinkles, etc.). It may help identify medication alternatives for patients if there are issues with cost, availability, or clinical response.
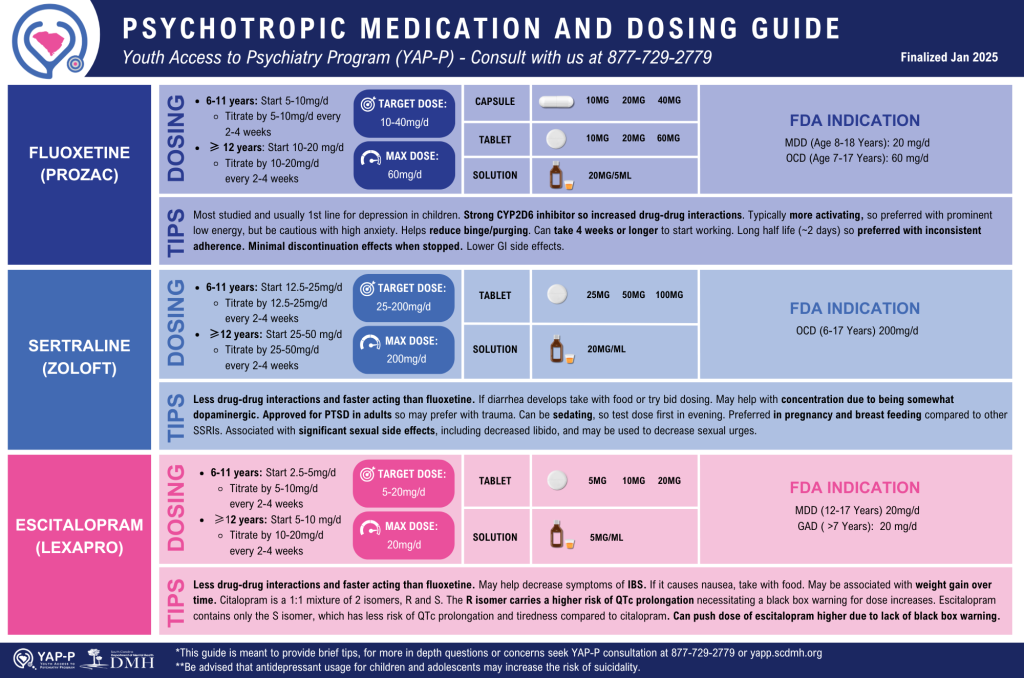
Developed by YAP-P consultant, Dr. Khetpal, this guide’s intended purpose is for antidepressant dosing guidance. The guide shows medication (fluoxetine, sertraline, escitalopram, duloxetine, bupropion, & mirtazapine), method of administration, target dose, maximum dose, FDA indications, and tips.
Trauma ScreenTIME Pediatric Primary Care Course
The ScreenTIME course equips professionals in child-serving systems with best practices for trauma screening. Designed to support early identification of traumatic stress in children, the course helps child-serving staff identify and support children suffering from traumatic stress as early as possible and connect those in need with effective services.
School Mental Health Quality Guide on Screening
Part of a collection of resources developed by the National Center for School Mental Health (NCSMH) at the University of Maryland School of Medicine, this guide contains background information on school mental health screening in addition to best practices, possible action steps, examples from the field, and supplemental resources.
Mental Health Screening Tools for School Settings
This resource provides an overview of screening in the schools and considerations for screening in the school setting. It also includes a curated list of sample tools that can be administered by students, educators, or parents.
American Academy of Pediatrics (AAP)’s Bright Futures Toolkit: Links to Commonly Used Screening Instruments and Tools includes tools for use during Bright Futures visits as well as screening and assessment tools for use at the discretion of the health care professional.
American Academy of Pediatrics (AAP)’s Screening Technical Assistance and Resource (STAR) Center focuses on early childhood screening and offers a Screening Tool Finder to help identify appropriate tools for assessing child development, perinatal depression, and social drivers of health.
Massachusetts Child Psychiatry Access Program Primary Care Behavioral Health Screening Toolkit provides guidance on using standardized behavioral health screening tools in the primary care setting. It addresses clinical considerations, such as integrating screening into well-child visits and responding to elevated risk, and includes several MassHealth-approved tools.